Home > Blogs > Monitoring in High Flow Oxygen Therapy and Non-Invasive Ventilation: A Vital Aspect of Patient Care
Monitoring in High Flow Oxygen Therapy and Non-Invasive Ventilation: A Vital Aspect of Patient Care
- Published on:
Monitoring in High Flow Oxygen Therapy and Non-Invasive Ventilation: A Vital Aspect of Patient Care
- Published on:

On this page

High Flow Oxygen Therapy (HFOT) and Non-Invasive Ventilation (NIV) have revolutionised respiratory care by offering effective alternatives to invasive ventilation. However, ensuring patient safety and treatment success requires careful monitoring of respiratory parameters. Dr. Martin Dres from Sorbonne University recently presented at the European Society of Intensive Medicine Congress in Barcelona and offered some insightful perspectives on monitoring HFOT and NIV, highlighting the role of invasive and simple non-invasive techniques in predicting therapy outcomes. This month’s blog will look at the latest monitoring strategies and tools that enhance clinical decision-making for HFOT and NIV.
Monitoring of Tidal Volume (VT) during NIV
Expired tidal volume (VTe) is a simple yet effective metric for measuring treatment success when managing patients on NIV. Traditionally used in intubated patients, VTe has emerged as a valuable predictor for NIV patients as well.
A key study, “Failure of Non-invasive Ventilation for De Novo Acute Hypoxemic Respiratory Failure: Role of Tidal Volume” from Guillaume et al (1), measured the tidal volumes in two different patient categories: mild hypoxemia or moderate to severe hypoxemia. The study demonstrated that high expired tidal volumes are independently associated with NIV failure. In patients with moderate-to-severe hypoxemia, high expired tidal volumes (above 9.5 mL/kg predicted body weight) are associated with an increased risk of NIV failure. Similarly, another study by Jean-Pierre Frat (2) identified that tidal volume measured one-hour post-NIV initiation can predict NIV failure, with volumes above 9 mL/kg of PBW associated with higher risk.
Predictive Tools: ROX Index and VOX Index
For patients on High-Flow Oxygen Therapy (HFOT), measuring tidal volume is not possible, so researchers have proposed innovative solutions. A notable approach is from Cheng et al. (3), who reported an approach to measuring TV generated by patients supported with HFOT and established a novel index named VOX (Volume-OXygenation) based on VT to predict HFNC failure in patients with acute hypoxemic respiratory failure (AHRF).
The VOX index (adapted from the ROX index which we will discuss later) combines SpO2/FiO2 over VT—to evaluate the patient’s respiratory drive. The patient on HFOT would be placed on a trial of NIV solely to measure the tidal volume and use this figure to predict the outcome. The study suggests that VT is a better estimate of the early increase in respiratory drive compared with respiratory rate which forms the basis of the commonly used ROX index. This approach could enhance early intervention, improving patient outcomes in HFOT failure acute hypoxemic respiratory failure (AHRF).
Determining the appropriate timing for transitioning from spontaneous breathing HFOT to invasive mechanical ventilation (IMV) presents a significant challenge in the clinical management of patients with acute respiratory failure (ARF). HFOT may prevent the need for intubation in some ARF patients, however, it may cause unnecessary delays in the initiation of mechanical ventilation (MV) and worsen clinical outcomes.
The ROX index (SpO₂/FiO₂ over respiratory rate) is an established tool for HFOT monitoring, thanks to its simplicity and bedside application. Proposed by Roca et al (4), this method has been validated to predict the risk for endotracheal intubation (5). You can read more about the ROX index in our previous blog post: The Highs And Lows Of The ROX Index | Inspire Blog
The ROX index (Respiratory rate and OXygenation) gives an indication of who is going to succeed or fail on HFOT.
A ROX index greater than or equal to 4.88 assessed at 2, 6, and 12 hours is indicative of high-flow success and correlates with a reduced likelihood of intubation. ROX index values that fall over time can signal the need for intervention, helping clinicians respond swiftly to deteriorating respiratory function. In patients with ARF and pneumonia, the ROX index can identify patients at low risk for HFOT failure in whom therapy can be continued after 12 hours.
The ROX index is a ratio and simple to monitor, however, even though the respiratory rate can indicate increased respiratory drive, it is not overly sensitive to slight early changes. Respiratory rate may not increase much in response to early changes in respiratory drive, thereby reducing the ROX index’s capacity to detect early indicators of deteriorating respiratory health.
In combination, these tools—ROX and the newly proposed VOX index—provide a holistic assessment framework, adapting well to the varied dynamics of HFOT and NIV.
The Role of Advanced Monitoring: Oesophageal Balloon
Additionally, Dr. Martin Dres discussed the more advanced monitoring methods for patients experiencing severe respiratory failure. Specifically highlighting a study from Italy (6), exploring the hypothesis that inspiratory effort might be a major determinant of NIV failure in these patients. A thorough assessment of inspiratory effort can be obtained through oesophageal manometry. Research has shown that respiratory decompensation and the risk of lung damage are associated with an increase in inspiratory pressures.
This study measured changes in chest pressure using a specialised nasogastric tube (NutriVent) which included a pressure sensor and was inserted before initiation of NIV. The nasogastric tube was attached to a device that measured pressure changes at the end of exhalation. However, the complexities of oesophageal manometry prevent its widespread usage.
The Role of Dyspnoea Scales in Patient Monitoring Tools
The American Thoracic Society (ATS) state that up to 50% of patients admitted to acute, tertiary care hospitals and 25% of patients seeking care in ambulatory settings experience dyspnoea, a common and frequently debilitating symptom. Dyspnoea, one of the most distressing experiences, observed in 35–50% of mechanically ventilated patients, whether they receive invasive mechanical ventilation or NIV. (7)
When predicting a patient’s clinical course, dyspnoea is a powerful predictor of mortality that frequently surpasses standard physiological measurements. High dyspnoea levels shortly after beginning NIV are associated with a higher risk of NIV failure, particularly in COVID-19 cases and for patients on NIV, moderate-to-severe dyspnoea early on is associated with higher mortality and longer ICU/hospital stays (8).
According to the ATS definition, dyspnoea is “a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intent.” Because dyspnoea is a symptom (i.e., the sense of an abnormal or unpleasant internal state), it is necessary to distinguish it from signs like tachypnoea, intercostal retractions, and the use of accessory muscles that doctors typically use as indicators of respiratory distress. (7)
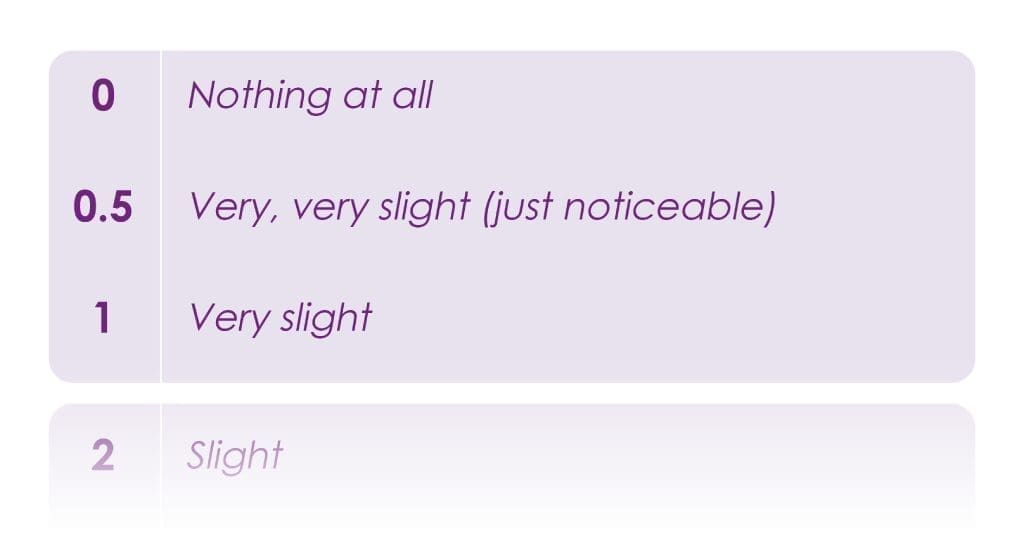
The Borg scale (0–10), a simple tool with verbal descriptors linked to specific numbers, allows communicative patients on HFOT or NIV to rate their breathlessness (9). This scale effectively captures how breathing feels to the patient, offering a category-based assessment with ratio-like properties. According to ERS-ESICM, the Borg scale is surprisingly accurate as a subjective measure, making it a valuable addition to patient monitoring tools. (8)

Monitoring and Decision-Making: Toward an Integrated Approach
Close monitoring is essential in High Flow Oxygen Therapy (HFOT) and Non-Invasive Ventilation (NIV) to support timely clinical decisions and improve patient outcomes. Tools like the ROX and VOX indices, alongside measures like tidal volume and dyspnoea scales, provide valuable insights into respiratory function and therapy success. Advanced methods, such as Esophageal manometry, offer deeper understanding in severe cases, though simpler, non-invasive techniques remain practical and widely accessible.
As monitoring strategies continue to evolve, these tools enable clinicians to detect early signs of deterioration, improving respiratory care. By integrating advanced and accessible monitoring approaches, healthcare providers can better tailor interventions, reducing the need for invasive ventilation while ensuring the best possible outcomes for patients with HFOT and NIV.

Abby Lennon
Clinical Nurse Adviser
References
- Carteaux, Guillaume et al Failure of Noninvasive Ventilation for De Novo Acute Hypoxemic Respiratory Failure: Role of Tidal Volume*. Critical Care Medicine 44(2):p 282-290, February 2016. | DOI: 10.1097/CCM.0000000000001379 Critical Care Medicine
- Frat, Jean-Pierre MD et al. Predictors of Intubation in Patients With Acute Hypoxemic Respiratory Failure Treated With a Noninvasive Oxygenation Strategy*. Critical Care Medicine 46(2):p 208-215, February 2018. | DOI: 10.1097/CCM.0000000000002818. Critical Care Medicine
- Chen D, Heunks L, Pan C, Xie J, Qiu H, Yang Y, Liu L. A Novel Index to Predict the Failure of High-Flow Nasal Cannula in Patients with Acute Hypoxemic Respiratory Failure: A Pilot Study. Am J Respir Crit Care Med. 2022 Oct 1;206(7):910-913. doi: 10.1164/rccm.202203-0561LE. PMID: 35671485; PMCID: PMC9799263. A Novel Index to Predict the Failure of High-Flow Nasal Cannula in Patients with Acute Hypoxemic Respiratory Failure: A Pilot Study – PMC
- Roca et al, An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am J Respir Crit Care Med. 2019 Jun 1;199(11):1368-1376. doi: 10.1164/rccm.201803-0589OC. PMID: 30576221. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy | American Journal of Respiratory and Critical Care Medicine
- Roca et al, Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index,Journal of Critical Care, Volume 35, 2016,Pages 200-205, ISSN 0883-9441, https://doi.org/10.1016/j.jcrc.2016.05.022. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index – ScienceDirect
- Tonelli R, Fantini R, Tabbì L, Castaniere I, Pisani L, Pellegrino MR, Della Casa G, D’Amico R, Girardis M, Nava S, Clini EM, Marchioni A. Early Inspiratory Effort Assessment by Esophageal Manometry Predicts Noninvasive Ventilation Outcome in De Novo Respiratory Failure. A Pilot Study. Am J Respir Crit Care Med. 2020 Aug 15;202(4):558-567. doi: 10.1164/rccm.201912-2512OC. PMID: 32325004; PMCID: PMC7427381. Early Inspiratory Effort Assessment by Esophageal Manometry Predicts Noninvasive Ventilation Outcome in De Novo Respiratory Failure. A Pilot Study – PMC
- Parshall, M. B., Schwartzstein, R. M., Adams, L., Banzett, R. B., Manning, H. L., Bourbeau, J., Calverley, P. M., Gift, A. G., Harver, A., Lareau, S. C., Mahler, D. A., Meek, P. M., & O’Donnell, D. E. (2012). An Official American Thoracic Society Statement: Update on the Mechanisms, Assessment, and Management of Dyspnea. American Journal of Respiratory and Critical Care Medicine, 185(4), 435–452. https://doi.org/10.1164/rccm.201111-2042st
- Demoule, A., Decavele, M., Antonelli, M. et al. Dyspnoea in acutely ill mechanically ventilated adult patients: an ERS/ESICM statement. Intensive Care Med 50, 159–180 (2024). https://doi.org/10.1007/s00134-023-07246-x