Positive End-Expiratory Pressure (PEEP): Understanding Its Role
- Published on:
Positive End-Expiratory Pressure (PEEP): Understanding Its Role
- Published on:
On this page
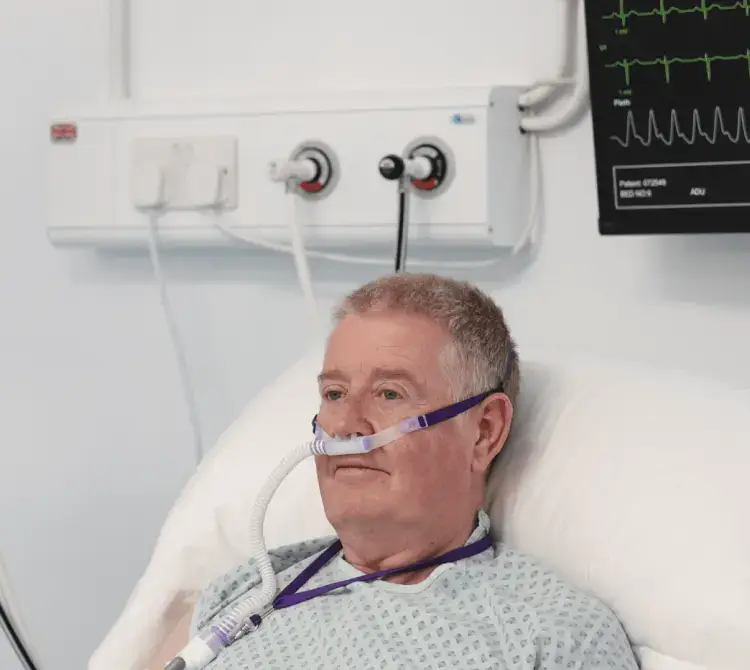
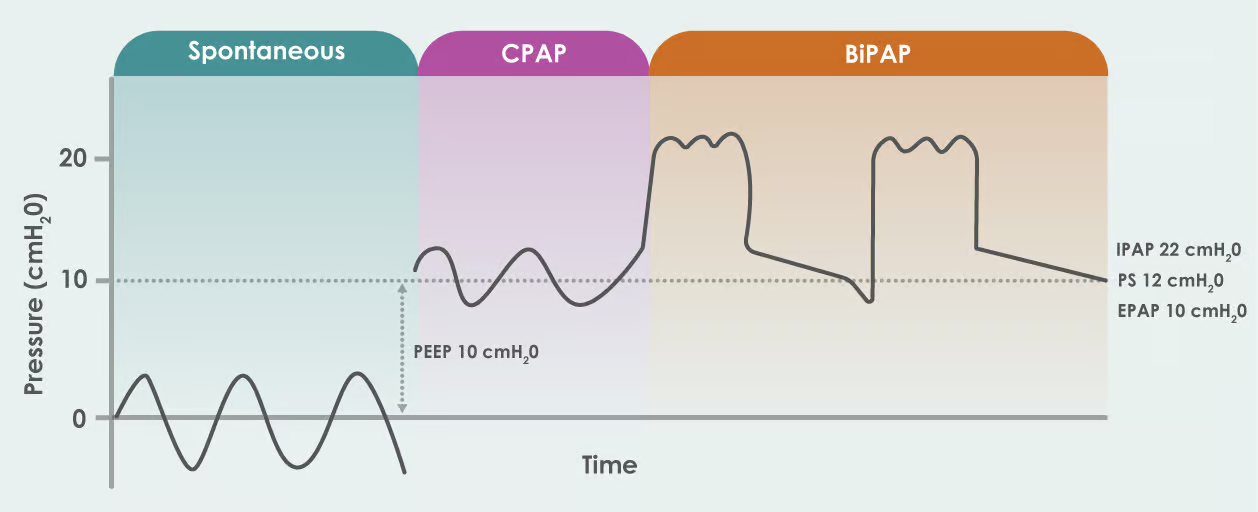
Positive end-expiratory pressure (PEEP) is a parameter that can be set in patients receiving either invasive or non-invasive mechanical ventilation (NIV). On a flow driver, such as the AquaVENT® FD140i, PEEP is introduced to the breathing circuit via a PEEP valve. In contrast, on a ventilator, PEEP can either be an adjustable setting (extrinsic PEEP) or an unintended consequence due to air trapping (auto PEEP). Typically, during face mask NIV and CPAP, PEEP ranges from 5 cmH2O to 8 cmH2O, while pressure support is set between 7 cmH2O and 14 cmH2O (1,3).
Understanding PEEP
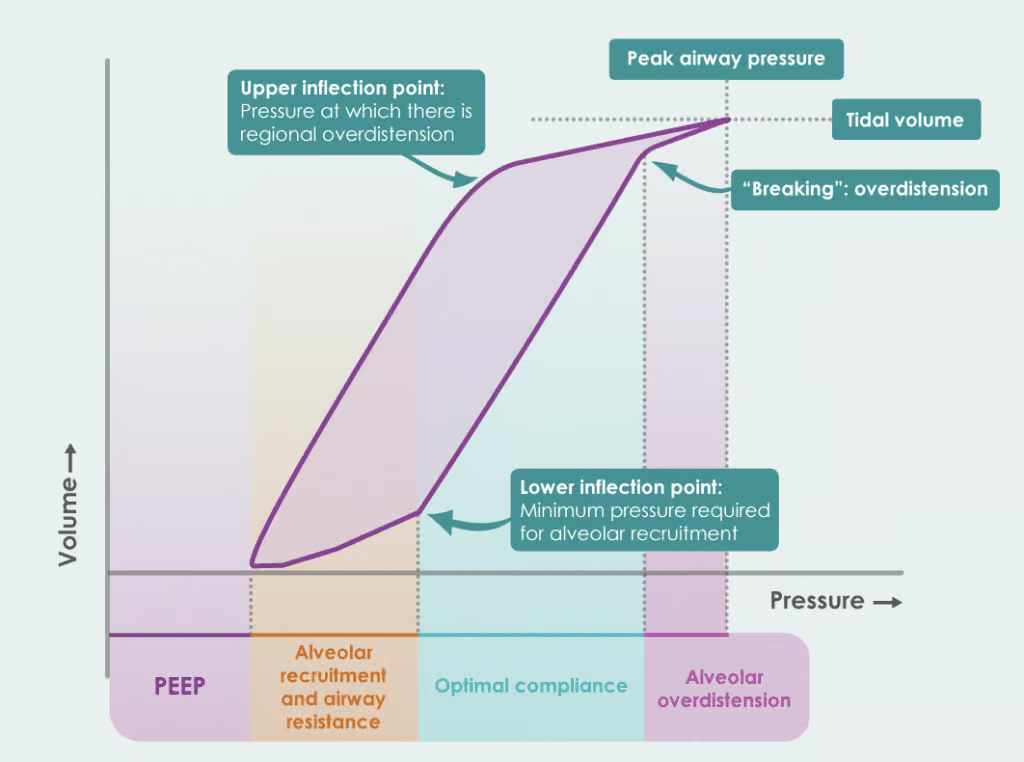
When describing PEEP in their 2016 guidelines, the British Thoracic Society (2) highlight that this area of physiology can cause confusion among healthcare professionals and the optimal method for setting it remains debated. They explain, PEEP helps shift the lungs to a more compliant part of the pressure-volume curve, meaning the lungs require less pressure to expand, making breathing more efficient.
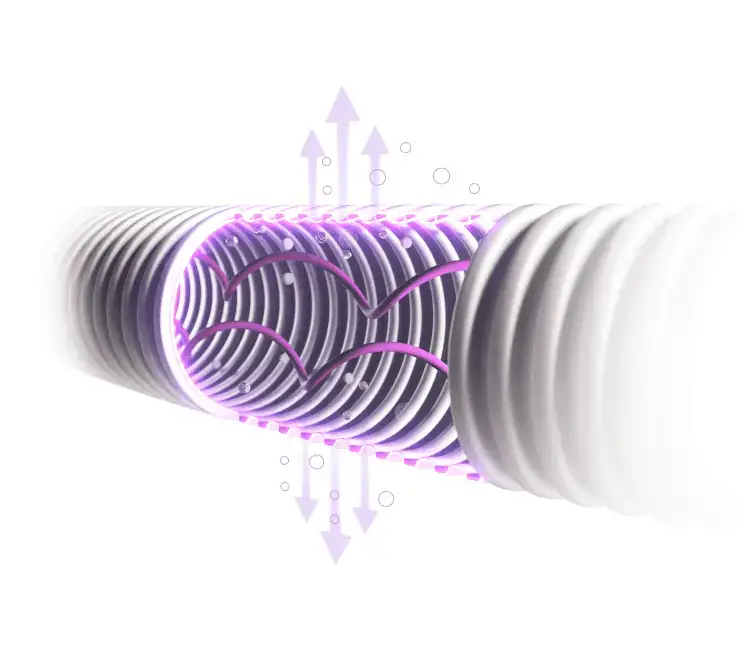
Lungs never completely empty; they retain some air, known as Functional Residual Capacity (FRC), or intrinsic PEEP. This remaining pressure at the end of exhalation prevents lung collapse and helps keep the alveoli open. When you breathe in, the negative pressure in the pleural space (-5 cmH2O) maintains a small amount of air in the lungs (+5 cmH2O), which is counteracted by the positive pressure, keeping the lungs in a “rest state” until the diaphragm contracts (4).
Modes of non-invasive ventilation
- variable flow with two levels of pressure (e.g. BiPAP).
- continuous flow with a continuous level of pressure (e.g. CPAP)
In BiPAP therapy, two parameters are set: Inspiratory Positive Airway Pressure (IPAP) and Expiratory Positive Airway Pressure (EPAP).
IPAP (Inspiratory Positive Airway Pressure):
- Applied during inhalation to help push air into the lungs, making it easier to breathe in.
- Main function: Supports ventilation, increases tidal volume, and removes CO₂.
EPAP (Expiratory Positive Airway Pressure):
- Applied during exhalation, similar to PEEP, to keep the airways open.
- Main function: Reduces airway closure, improves oxygen levels, and prevents alveolar collapse.
Key Difference:
- IPAP helps with inhalation, reducing effort and removing CO₂.
- EPAP aids exhalation, keeping airways open and improving oxygenation (6).
This mode of ventilation is a common choice for patients with hypercapnic respiratory failure, COPD and sleep disorders such as obstructive sleep apnoea (OSA). By splinting the upper airways and assisting respiratory muscles during inspiration, BiPAP reduces the work of breathing and dyspnoea (7,8).
Continuous Positive Airway Pressure (CPAP) provides a continuous, fixed positive pressure throughout the entire breathing cycle. Unlike BiPAP, CPAP does not assist with inhalation but maintains steady pressure to prevent airway collapse and support lung volume. CPAP is traditionally delivered via a high-flow generator, such as Venturi systems or air/oxygen blenders (e.g., AquaVENT® FD140i), which supplies fresh gas through an inlet port, with an adjustable PEEP valve in the breathing circuit. Its simplicity makes CPAP a cost-effective solution in emergency settings and easy to use outside intensive care, as it does not require a ventilator (3).
CPAP is often chosen for patients with acute hypoxic respiratory failure, pneumonia, or pulmonary oedema, where lung compliance is low, and the lungs become stiff, or fluid filled. This leads to ineffective alveolar ventilation, meaning the lungs cannot exchange gases efficiently (9).
CPAP increases airway pressure, improves arterial oxygenation, increases end-expiratory lung volume, and improves cardiac function by reducing left ventricular afterload and right ventricular preload, ultimately decreasing inspiratory effort and the work of breathing (10). Continuous PEEP helps keep alveoli open, preventing collapse and increasing the amount of air remaining in the lungs after exhalation (FRC). By increasing FRC, CPAP allows more oxygen to remain in the lungs between breaths (6).
Conclusion
The balance of PEEP settings is critical for effective patient care. Insufficient PEEP can lead to low oxygen levels or airway collapse, while excessive PEEP can cause lung damage, air trapping, pneumothorax, and potentially lead to cardiac complications such as hypotension or right ventricular failure. (3) High PEEP levels can also increase intracranial pressure and contribute to fluid retention. Given these risks, it’s essential to find the optimal PEEP setting for each patient in critical care. These settings are typically guided by clinical judgment, carefully weighing the dangers of hyperinflation versus inadequate oxygenation. Continuous patient monitoring is key to identifying early signs of treatment failure, preventing delayed intubation, and ensuring effective protective ventilation. (11)

Abby Lennon
Clinical Nurse Adviser, RN
Abby works alongside the Clinical Education Team to provide support and education to healthcare professionals using her knowledge and experience as a registered nurse working in respiratory wards and intensive care units over the last eight years.
References
- Mora, A.L. and Mora, J.I. (2019). Positive end-expiratory pressure (PEEP). [online] National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK441904/.
- Davidson, A.C. (2016). BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax, 71(Suppl 2), pp.ii1–ii35. doi:https://doi.org/10.1136/thoraxjnl-2015-208209.
- Rosà, T., Menga, L.S., Tejpal, A., Cesarano, M., Michi, T., Sklar, M.C. and Grieco, D.L. (2022). Non-invasive ventilation for acute hypoxemic respiratory failure, including COVID-19. Journal of Intensive Medicine, [online] 3(1). doi:https://doi.org/10.1016/j.jointm.2022.08.006.
- Acosta, P., Santisbon, E. and Varon, J. (2007). ‘The Use of Positive End-Expiratory Pressure in Mechanical Ventilation’. Critical Care Clinics, 23(2), pp.251–261. doi:https://doi.org/10.1016/j.ccc.2006.12.012.
- D.Roth, J.Mayer, W.Schreiber. Acute carbon monoxide poisoning treatment by non‐invasive CPAP‐ventilation, and by reservoir face mask: Two simultaneous cases. American Journal of Emergency Medicine 36, Issue 9.
- The Royal Marsden NHS Foundation Trust. (2020). The Royal Marsden manual of clinical and cancer nursing procedures (10th ed.). Wiley. https://www.rmmonline.co.uk/
- Vargas M, Marra A, Vivona L, Ball L, Marinò V, Pelosi P, Servillo G. Performances of CPAP Devices With an Oronasal Mask. Respir Care. 2018 Aug;63(8):1033-1039. doi: 10.4187/respcare.05930. Epub 2018 May 29. PMID: 29844211.
- Demoule A, Hill N, Navalesi P. Can we prevent intubation in patients with ARDS? Intensive Care Med. 2016 May;42(5):768-771. doi: 10.1007/s00134-016-4323-6. Epub 2016 Mar 23. PMID: 27007110.
- D.Stickle. BiPAP noninvasive ventilation for COPD. Journal for Respiratory Care Practitioners 2018.
- Munshi L, Mancebo J, Brochard LJ. Noninvasive Respiratory Support for Adults with Acute Respiratory Failure. N Engl J Med. 2022 Nov 3;387(18):1688-1698. doi: 10.1056/NEJMra2204556. PMID: 36322846.
- Millington, S.J., Cardinal, P. and Brochard, L. (2022). How I Do It: Setting and Titrating Positive End Expiratory Pressure. Chest, 161(6).